Advertisement|Remove ads.
Humana To Slash Red Tape Around Prior Authorization For Care Services By 2026: Retail Remains Optimistic

Humana Inc. (HUM) on Tuesday announced measures aimed at accelerating prior authorizations for care services, particularly outpatient services such as colonoscopies and CT scans.
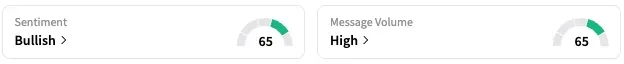
On Stocktwits, retail sentiment around Humana trended within ‘bullish’ territory, accompanied by ‘high’ message volume.
The actions, the health insurance company said, will reduce the number of prior authorization requirements and make the process faster and more seamless while preserving the system of checks and balances that ensures the most high-cost, high-risk treatments are reviewed and approved before care is delivered.
Humana CEO Jim Rechtin said that the current healthcare system is “too complex, frustrating, and difficult to navigate,” while emphasising the need to “do better.”
“We are committed to reducing prior authorization requirements and making this process faster and more seamless to better support patients, caregivers, physicians, and healthcare organizations,” he added.
By the start of 2026, Humana will eliminate approximately one-third of prior authorizations for outpatient services and provide a decision within one business day on at least 95% of all complete electronic prior authorization requests. Currently, Humana provides a decision within one business day on more than 85% of outpatient procedures.
Humana will remove the authorization requirement for diagnostic services, including colonoscopies and transthoracic echocardiograms, as well as select CT scans and MRIs, by January 1, it said.
The company also announced that it will launch a new gold card program in 2026, which will waive prior authorization requirements for certain items and services for providers who have a proven record of submitting coverage requests that meet medical criteria.
Starting in 2026, the insurance provider will also report its prior authorization metrics to increase transparency. This includes prior authorization requests that are approved, denied, and approved after appeal, as well as the average time between submission and decision.
A Stocktwits user opined that while Humana stock has fallen as hard as its peer, UnitedHealth, it does not share the same stigma as UNH.
However, it is essential to note that UNH shares have dropped 44% this year.
Meanwhile, HUM stock is down 10% this year and approximately 41% over the past 12 months.
For updates and corrections, email newsroom[at]stocktwits[dot]com.









/filters:format(webp)https://news.stocktwits-cdn.com/large_Webull_stock_resized_jpg_48b42f4c8f.webp)
/filters:format(webp)https://news.stocktwits-cdn.com/jaiveer_jpg_280ad67f36.webp)
/filters:format(webp)https://st-everywhere-cms-prod.s3.us-east-1.amazonaws.com/large_Morgan_Stanley_resized_Mar_19_jpg_784f532fd2.webp)
/filters:format(webp)https://news.stocktwits-cdn.com/large_Getty_Images_2192180432_jpg_5a4c947a6a.webp)
/filters:format(webp)https://news.stocktwits-cdn.com/large_Getty_Images_2243967992_jpg_33943df3b8.webp)
/filters:format(webp)https://st-everywhere-cms-prod.s3.us-east-1.amazonaws.com/unnamed_jpg_9dff551b50.webp)
/filters:format(webp)https://news.stocktwits-cdn.com/Getty_Images_2197860201_jpg_c4f2083335.webp)
/filters:format(webp)https://news.stocktwits-cdn.com/Aashika_Suresh_Profile_Picture_jpg_2acd6f446c.webp)
/filters:format(webp)https://news.stocktwits-cdn.com/large_US_economy_representative_image_jpg_88c3aa4736.webp)